To qualify for a power mobility device with Medicare funding, physicians, nurse practitioners, physician’s assistants or clinical nurse specialists that are treating a patient for their mobility needs, must evaluate a patient for their power mobility needs and document the exam in their normal record-keeping format to meet Medicare’s guidelines for power mobility.
These guidelines can present a daunting task but working in tandem with a licensed certified medical professional- such as a physical or occupational therapist that is skilled in mobility evaluations, can make this a much easier process.
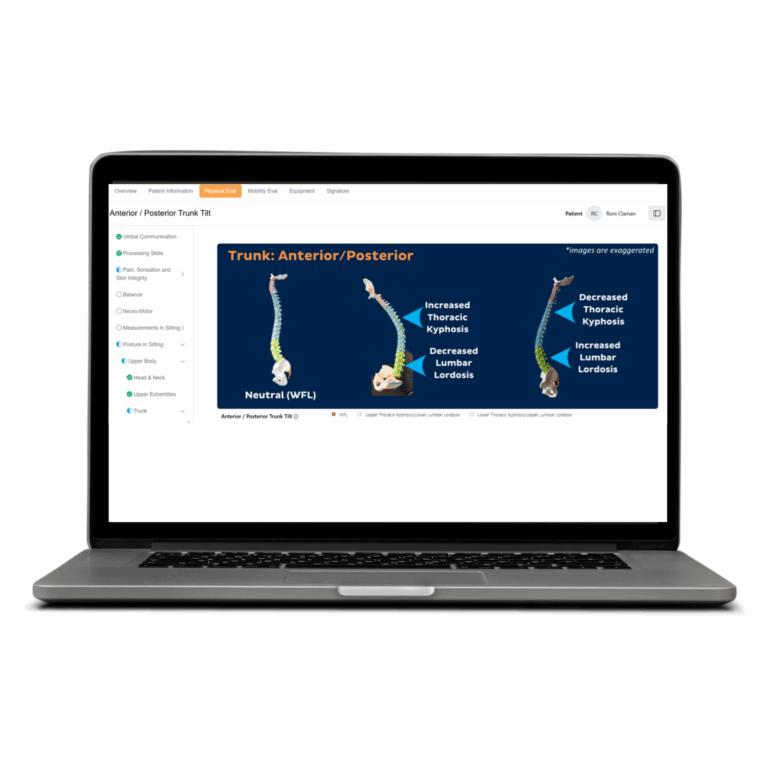
Working with a PT or OT to complete this examination, often referred to as a complete face to face for power mobility, can also present opportunities for duplication of effort. When examination findings are duplicated by both the physician and therapist, such as strength measurements, range of motion measurements and other objective tests, the findings can often be different. For example, a patient can present with 4+/5 upper extremity strength during a morning examination with their physician and then, perhaps days or even weeks later, present with 3/5 upper extremity strength when tested by their PT or OT during an afternoon or evening evaluation. This can introduce conflicting information in the complete face to face and, as a result, the opportunity for denials from CMS and other payers that follow CMS guidelines.
How Can These Denials Best Be Avoided?
1. Doctors: don’t be afraid to be subjective – at least with some parts of your exam documentation.
When you are referring to a therapist to complete part of the mobility evaluation process there will be a full report containing detailed strength measurements, range of motion measurements and other objective findings to support subjective statements that you make. For example, something like “patient has marked weakness of his/her bilateral upper extremities.” As long as the objective findings from the therapist, that you are stating your concurrence and signing/dating into the complete face to face record, correlate with the subjective statements that you provide, no conflicting information denials should result.
2. Double-check the “normal” statements.
Most EMR and EHR systems default to “normal” statements and must be overridden to state abnormal findings. Statements such as, “patient is ambulatory and walked into clinic today” or “ambulatory status: normal” can be considered conflicting information when reviewed against the balance of the medical documentation.
3. It’s important to note that Medicare expects the physician, nurse practitioner, physician’s assistant or clinical nurse specialist that is conducting the face to face exam for power mobility to complete the following:
- This visit must document the decision to prescribe a power mobility device.
- There must be a history and physical exam by the physician focusing on an assessment of their patient’s mobility limitation and needs on a typical day.
- The physician needs to document the examination in a detailed narrative note in their chart in the format that they use for other entries.
- It should contain as much objective data as possible; however, duplication of effort between the therapist’s evaluation and doctor’s exam (i.e., strength, range, etc.) is
- not required and when present, can conflict with the therapist’s mobility evaluation and introduce denial opportunities.
- The note must clearly indicate that a major reason for the visit was a mobility examination and provide the patient’s mobility-related diagnosis or diagnoses.
- The examination is customized, just like the patient’s complex rehab equipment, to the individual’s conditions. The physical examination is focused on the body system(s) that are responsible for the mobility limitation.
Remember, above all, that the examination findings presented by the physician and mobility evaluation documented by the therapist should work together, as a complete face to face record for power mobility, to paint a picture of the client’s functional abilities and limitations on a typical day. The better these two reports work together to support Medicare’s qualification guidelines, the fewer denials the client will experience, and ultimately, the faster the client will receive their new complex power mobility equipment.

author
Andria Pritchett
Corporate Compliance Officer – West Division; Executive Director of Compliance Training & Education
Andria Pritchett has been with Numotion since 2010. Prior to beginning her career in complex rehab technology, she was a practice administrator for a large multi-specialty therapy clinic. Upon shifting focus to complex rehab technology in 2010, Andria has used her extensive management, clinical and Medicare knowledge to develop and manage the traditional Medicare portion of many aspects of business at Numotion. She has managed Medicare Billing and Medicare Audits, ALJ Hearings, Funding and Order Processing, and took a very active role in the Medicare education program within Numotion. As a current committee member for Medicare Jurisdiction D DME MAC Advisory Committee – Rehab A Team, this vital role allows her to stay on top of the reimbursement environment and educate both internally and externally at the highest level. Andria currently develops a wide range of curriculum and educates Numotion leadership, ATPs and external clinicians nationally on a variety of topics.