“Letter of medical necessity” – are words that can initiate fear and confusion in many a therapist. But do they need to?
When I was in third grade, our teacher required us to write down detailed steps of how to make a peanut butter and jelly sandwich. I wrote, “put the peanut butter on one piece of bread. Put the jelly on the other piece of bread. Put pieces of bread together.” My teacher then followed my instructions by putting the jar of peanut butter on top of one piece of bread, the jar of jelly on top of another, then carefully slid the two slices of bread to touch. I learned my lesson. The devil is in the details.
While you may assume that a person with two leg amputations is unable to walk, or someone with a C4 spinal cord injury would not be able to propel a wheelchair manually, insurers assume no such thing – and, good for them. They know humans are amazing creatures, and some people defy the odds. It is up to you to explain to your unique client, and to paint the picture of medical necessity.
Where Did This Start?
According to Bergthold (1995), the concept of medical necessity was born to ensure that hospitals and physicians received payment as private insurances began to be developed. They initially routinely covered what a physician decided was medically necessary without questioning. Throughout the 1960s, the judgment of a physician continued to be the gold standard of what was medically necessary. During the 1970s, as medical costs continued to rise, private insurances began to require physicians to justify medical necessity. In the 1980s, the RAND Corporation started to order studies to evaluate the efficacy of certain medical procedures to analyze medical necessity.
Beginning in the 1990s, a typical definition of medical necessity looked like this; Services or supplies which are required for treatment of illness, injury, diseased condition, or impairment and are consistent with the patient’s diagnosis or symptoms; appropriate treatment according to generally accepted standards of medical practice; not provided only as a convenience to the patient or provider; not investigational or unproven; not excessive in scope, duration or intensity; provided at the most appropriate level of service that is safe. (Bergthold, 1995, p.183)
Some even included the term “not more-costly than alternative services,” with the overriding concept of preserving scarce resource.
Back to the question of the Letter of Medical Necessity (LMN). As part of a thorough seating and mobility evaluation, it is:
- A tool to preserve scarce resources
- A document to define what is necessary as the least costly option to meet medical needs
- Written to give the insurer a clear picture and understanding of the person in need
A record of your treatment plan. With a seating evaluation, your treatment plan is the application of equipment to your client.
What is My Role?
As the author of the LMN, you are the artist. You must paint the details of function in such a way that the reader can explicitly imagine the abilities of your client. Unfortunately, when you are new to the process, this may take much time and attention. For those of you who are skeptical, I assure you that it WILL get easier.
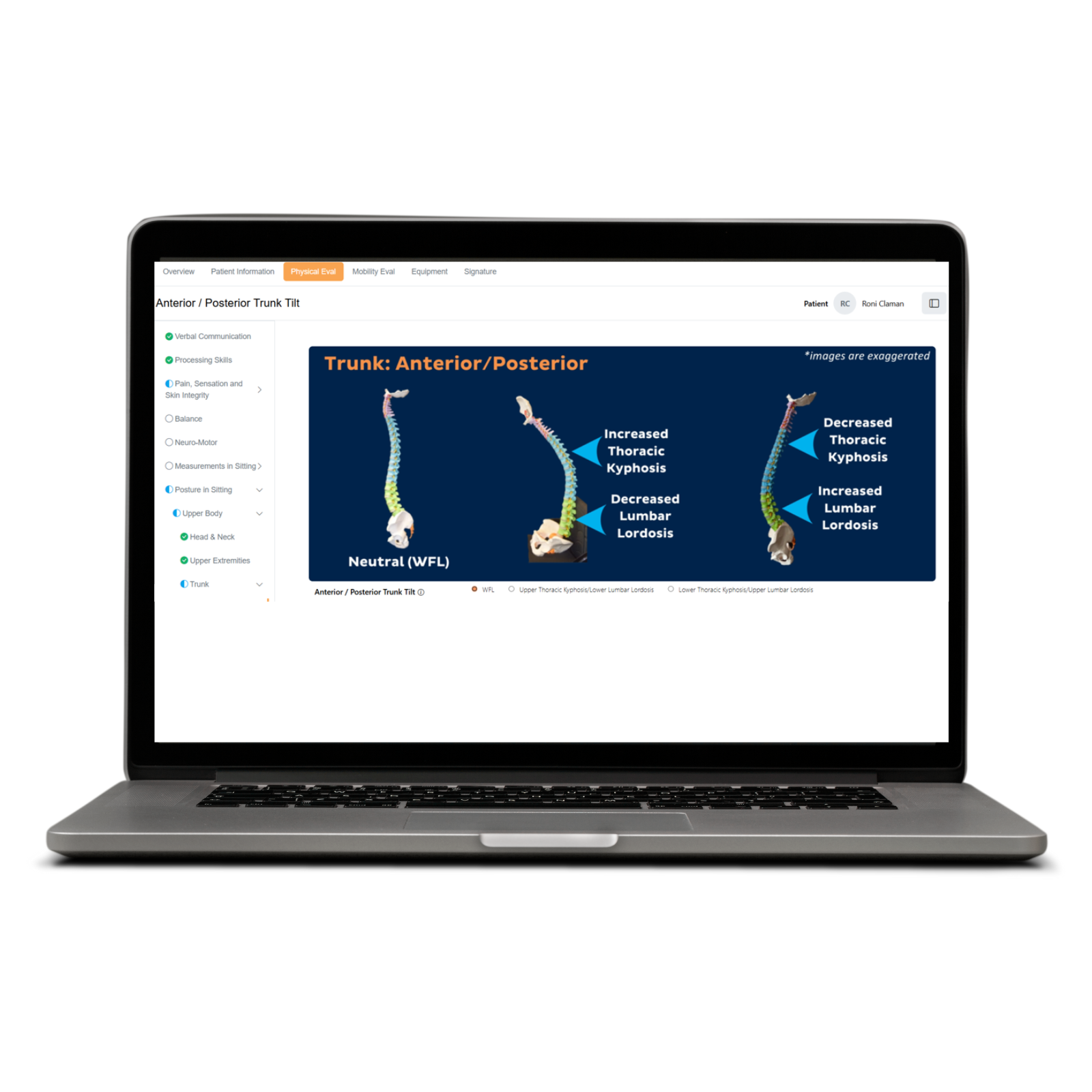
Following are a few things that are easily missed that will make that picture much more vibrant to documentation reviewers. Always remember the goal is to provide your client access to mobility-related activities of daily living (MRADL’s) in a safe and timely manner. The information collected in a seating and mobility evaluation is no different than most therapy evaluation. The “treatment plan,” or plan of care, instead of being treatment, such as balance training, is the equipment recommended.
You are stating the “why” of the equipment chosen. That’s why it is so important to define what that equipment will do for your client.
Rule Out Lesser Costly Items
What constitutes lesser costly? For mobility, start with the basics. Can your client use a cane, crutch, or walker? Make this the background of your portrait – your sky, your grass. Start with broad, graceful strokes of brief detail. This coverage will become like second nature as you do more of these letters. If you are asking for a power wheelchair, still address these, even if it should be clear why your client cannot utilize them.
Now a little more detail. Pepper your painting with some happy little trees. Can your client use a basic manual wheelchair (K0001)? A light-weight wheelchair (K0002, K0003, K0004)? An ultralight wheelchair (K0005)? Take a bit of time to answer why. The ATP with whom you are working can provide information about these types of equipment that will assist you in ruling out what is not appropriate and then justifying what is appropriate.
Now detail what best suits your client. Use that tiny little brush here.
Remember the Objective Measurements
Now we must paint the mountains. The poignant peaks of focus – the objective measures. While the person reading your LMN may have little experience testing for range of motion, balance, function, or strength, these must be included. These are the focal points of the client assessment. The strong facts on which your clinical assessment of needs are built. Do not gloss over the hard work you have done in finding what equipment best suits your client. Boldly paint the portrait.
If your client has impaired balance or endurance, what is better than a concrete number to substantiate what your clinical eye already sees?
“Weakness” is a weak substantiation. “Decreased balance” decreases your clients’ chance of getting the equipment they need. Use a Berg, use manual muscle testing (MMT) and range of motion (ROM), use a Tinetti, use a TUG, use a 6-minute walk/wheel test.
Why can your client not use something that is lesser costly? Use your resources (some below) and use the objective measures that best highlight your client’s needs.
You Know It – Share It!
Happy little clouds, blissful birds, bright sun rays. The details of the equipment, from the seating to the straps. You are almost done! The portrait has gained life, and now every little detail not only adds to your letter, but it also adds to the perfection of the equipment you have prescribed. You are the author. You know your client.
Freely share why you think each part of that equipment is perfect for your client. The person making determinations cannot see your client, so you must be the bridge to imagining that person that function.
Carefully and thoroughly build your peanut butter and jelly sandwich. Paint the background, paint the trees, and paint those beautiful details.
“This is your world. You’re the creator. Find freedom on this canvas Believe that you can do it, ‘Cuz, you can do it. You can do it.” – Bob Ross
If you have questions about writing LMN, or would like to learn more, contact me at alexis.rush@numotion.com.

author
Alexis Rush
OTR/L, ATP
Alexis Rush is an Assistive Technology Professional specializing in equipment for persons with spinal cord and brain injuries. She graduated from Xavier University with a degree in occupational therapy in 2003 and has her Doctor of Occupational Therapy from the University of St. Augustine. As a therapist, Alexis specialized in acute adult neurologic injury but also worked as a pediatric home health occupational therapist. She now works as a wheelchair provider at a large rehabilitation hospital in Denver, Colorado. Alexis is a mountain sports lover and an avid world explorer.
Resources:
Wheelchair Specific Tests: https://www.sralab.org/rehabilitation-measures/4-functional-tasks-wheelchairs
Wheelchair Skills Program: www.wheelchairskillsprogram.ca
Fillable Wheelchair Eval Form: https://www.numotion.com/Numotion/media/CoverageMaps/Houston- Methodist-fillable_1218.pdf
Nudigests and other resources: https://www.numotion.com/medical-professionals/document-library
References:
Bergthold, L. A. (1995). Medical necessity: Do we need it? Health Affairs, 14(4), 180-190.