Prescribing the right type of wheelchair can be challenging. Prescribing the optimal piece of equipment can improve the function and quality of life for an individual.
The right mobility device facilitates psychosocial and physical well-being. Prescribing the incorrect equipment can lead to fatigue, pain, loss of independence, poor quality of life and equipment abandonment. Clinicians and suppliers are charged with identifying the least costly mobility equipment that fully meets a user’s medical needs. Documentation of the clinical findings matched to the appropriate equipment is a clinician’s most powerful tool in advocating for their client’s independence and participation in a fulfilling life.
Power wheelchairs are classified by groups. At the end of this document is a reference guide that will help to identify the features that are necessary for your client’s mobility needs. Specific groups have different client functional requirements depending on the insurance.
How to Document
According to Dicianno & Tovey, 2007, a letter of medical necessity for a power wheelchair should contain the specific mobility limitations, how they affect ADL and IADL performance and why lesser-costly mobility devices (cane, walker, manual wheelchairs, or scooter) cannot appropriately provide mobility for the client. A full mobility assessment of abilities and limitations as well as prior trials of equipment should be detailed. Mobility examination should cover transfers, ambulation, ability to propel a manual wheelchair and ability to operate a power wheelchair, including safety, timeliness and quality as it relates to ADLs (Arledge et al., 2011). Even when one might assume that a mobility impairment is obvious based on the diagnosis, it is imperative to paint the whole picture. For example, why can a person not use a cane or crutch or walker? One must also rule out an optimally configured manual wheelchair. Especially if your client has arm movement, why is their manual wheelchair mobility or weight shifts not sufficient? Can they get to the toilet in timely fashion? Does manual wheelchair mobility place them at undue risk for musculoskeletal or tissue injury? Does fatigue over the course of a day prevent them from engaging in self-care activities at the end of a day?
Painting an accurate and complete picture is imperative to the success of mobility device documentation.
Insurers depend on the clinician to help them understand the why. When clinical notes state a patient can propel a manual wheelchair, a clinician must explain that:
- the client is only able to tolerate a manual wheelchair for 2 hours while he can stay up for 8 hours in a power wheelchair
- a power wheelchair for that client reduces the need for paid caregivers
When clinical notes state a patient can stand, a clinician must clarify:
- why standing is not a safe and reliable method of pressure relief
- why standing cannot be used to accomplish ADL’s
The client should engage in a trial of demonstration equipment that is as close to optimal as possible. This will allow the clinician, client and supplier to observe and document the impact of the prescribed equipment (Arledge et al., 2011). Thorough documentation allows the insurers to see what we see and agree with our findings.
Once all lesser costly options have been successfully ruled out, a clinician may then document which power-operated vehicle (POV) (in Medicare language, a POV is a scooter), will fully meet their client’s medical needs. The table included on the next page provides a brief explanation of each. Deciding between a group 2 and group 3 power wheelchair without an immediate need for multiple powered seating functions can be challenging for a clinician. Some things to consider include:
What If a Client Only Requires Tilt?
Vibration-dampening suspension is an important aspect of a group 3 power wheelchair to consider. High magnitude and long duration low magnitude vibrations have been found to be harmful to the human body (Garcia-Mendez, et al., 2013). Wheelchair users are exposed to vibrations that exceed these standards on a daily basis with minimal ability to lower their exposure without limiting their functional independence (Requejo, Maneekobkunwong, McNitt-Gray, Adkins, & Waters, 2009). If the client is a full-time wheelchair user, what are the potential impacts of the constant encounters with thresholds and uneven surfaces they encounter on a daily basis? Can vibrations negatively impact hardware (such as spinal fusions)? What about pain or spasticity? How does this impact independence or even the ability to tolerate sitting in the chair for hours per day? If they cannot tolerate the chair, does it increase the need for caregiving services?
What If a Client Has a Progressive Neurologic Disease but Doesn’t Need the Group 3 Features…Yet?
Medicare covers group 3 power wheelchairs for all persons with a mobility-limiting neurologic diagnosis, congenital skeletal deformity or myopathy. Some private insurers want the documentation to explain why a group 3 is not appropriate. Group 3 power wheelchairs are modular, meaning you can add power seating functions and alternative drive controls later. A client with ALS may still be able to walk short distances, but in the lifetime of a power wheelchair (5 years minimum), that user will likely need an alternative way to drive other than a standard joystick. They will likely need power seating functions. While insurers do not cover items for future use, they do not want to purchase a new wheelchair prematurely. They will support the modularity of the group 3 power wheelchair when a client is likely to have a decline in function, as long as that prognosis is documented.
Advocating for the most appropriate power mobility device is crucial to a client’s independence. Knowing the functional differences between groups of power wheelchairs allows clinicians and suppliers to guide the prescription process as well as provide the least costly device that fully meets their client’s needs while keeping them safe. Accurately documenting need and ruling out inappropriate devices enables the insurance to understand the client’s function and provide the equipment that is tailored to each client’s needs.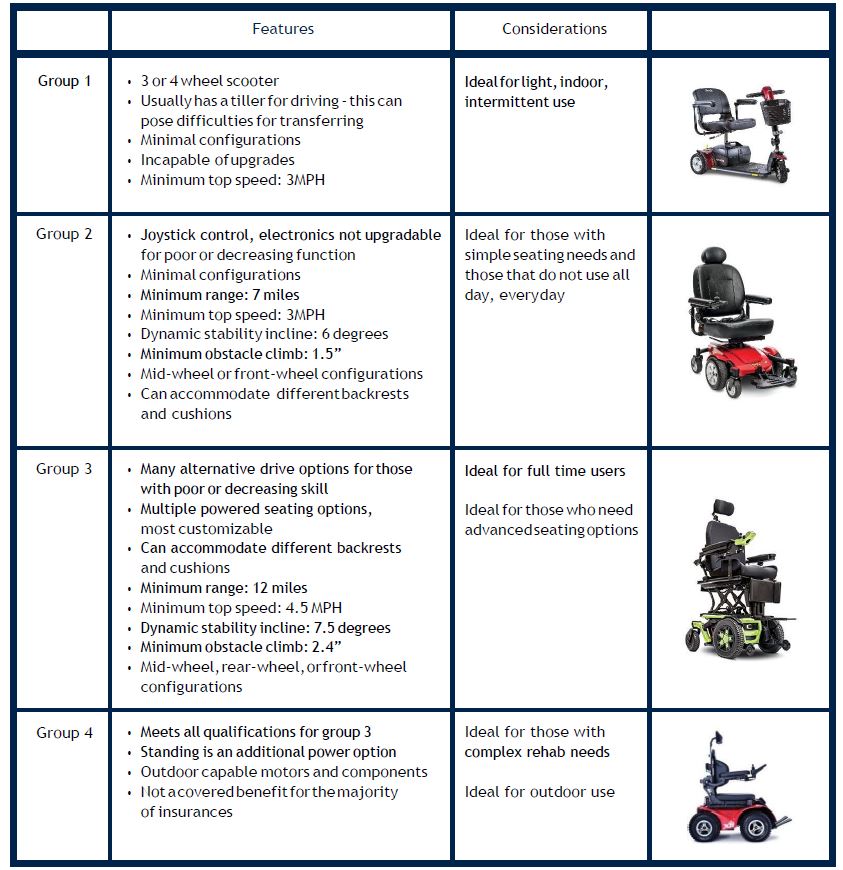

author
Alexis Rush
OTR/L, ATP
Alexis Rush is an Assistive Technology Professional specializing in equipment for persons with spinal cord and brain injuries. She graduated from Xavier University with a degree in occupational therapy in 2003 and has her Doctor of Occupational Therapy from the University of St. Augustine. As a therapist, Alexis specialized in acute adult neurologic injury but also worked as a pediatric home health occupational therapist. She now works as a wheelchair provider at a large rehabilitation hospital in Denver, Colorado. Alexis is a mountain sports lover and an avid world explorer.



